Statement on seasonal influenza vaccines for 2025–2026
Summary of NACI statement of April 30, 2025
On April 30, 2025, the Public Health Agency of Canada (PHAC) released the National Advisory Committee on Immunization's (NACI) Statement on seasonal influenza vaccines for 2025–2026. This guidance is based on current evidence and NACI expert opinion.
- Seasonal influenza vaccination is the most effective way to protect against influenza and its complications, including hospitalization and death.
- Every fall and winter, influenza and its complications place increased pressure on the healthcare system, especially as other respiratory viruses, such as COVID-19 and respiratory syncytial virus (RSV), circulate. In addition to protecting individuals against influenza and its complications, influenza vaccination helps reduce strain on healthcare resources during these peak seasons.
- Influenza vaccines that meet Health Canada's regulatory requirements for safety, efficacy, and quality are approved for use in Canada. Several types of influenza vaccines are authorized for use, including inactivated, recombinant, and live vaccines, some of which are targeted to specific age groups and health needs.
Following a thorough review of the evidence, NACI makes the following recommendations:
- Influenza vaccine should be offered annually to anyone 6 months of age and older who does not have a contraindication to the vaccine. Patients and providers should also be aware that risks of acquiring influenza are higher in some settings and risks from influenza infection are higher in some individuals than others. Immunization is particularly important for the following groups:
- People at high risk of severe disease, influenza-related complications, or hospitalization;
- All children 6 to 59 months of age;
- Adults and children with certain chronic health conditions;
- All pregnant women and pregnant individuals;
- All individuals of any age who are residents of nursing homes and other chronic care facilities;
- Adults 65 years of age and older; and
- Individuals in or from First Nations, Inuit, or Métis communities.
- People capable of transmitting influenza to those at high risk;
- Health care and other care providers in facilities and community settings;
- Household contacts, both adults and children, of individuals at high risk, whether or not the individual at high risk has been vaccinated;
- Those providing regular childcare to children 0 to 59 months of age, whether in or out of the home; and
- Those who provide services within closed or relatively closed settings to people at high risk (e.g., crew on a cruise ship).
- People who provide essential community services (including health care workers); and
- People whose occupational or recreational activities increase their risk of exposure to avian influenza A viruses (e.g., H5N1).
- People at high risk of severe disease, influenza-related complications, or hospitalization;
- Influenza vaccine should be offered as a priority to the groups for whom influenza vaccination is particularly important (listed above).
- The complete list of individuals at high risk for influenza-related complications or hospitalization, as well as those capable of transmitting influenza to these high-risk groups, can be found in the statement.
For the full statement, including supporting evidence and rationale, please see NACI's Statement on seasonal influenza vaccines for 2025–2026.
Download in PDF format
(256 KB, 6 pages)
COVID-19 & FLU VACCINE
TOP QUESTIONS ANSWERED ABOUT
COVID-19 AND INFLUENZA (FLU) IMMUNIZATION
Will the COVID-19 vaccine protect me against influenza (the flu)?
COVID-19 and influenza are two different viruses that cause two different illnesses. COVID-19 vaccines are designed to best protect you against the COVID-19 virus while the influenza vaccine is designed to best protect you against the flu. The COVID-19 vaccine is not designed to protect you against the flu.
There was hardly any flu last year so why should I get my flu shot this year?
According to experts and based on trends in the past, it is likely that this upcoming flu season might be much stronger and more widespread than the last one. The population’s overall immunity to the flu has declined over the COVID-19 pandemic because of lack of exposure to the latest flu strains. This means that more people might be at risk of getting the influenza virus when it returns. In the past there has been a strong increase in cases after a low outbreak season. Since distancing measures are being lifted, people are returning to offices, schools, public transit, restaurants, etc. This could mean a more widespread influenza outbreak and more severe flu epidemic and put our healthcare systems under significant pressure. In order to protect yourself from influenza, make sure you get your flu shot this year.
Can influenza trigger other non-respiratory illnesses?
Although influenza is primarily considered a respiratory infection, additional evidence suggests that influenza is associated with broader health complications. In fact, influenza can trigger severe cardiovascular complications. In the days following an influenza infection, the risk of heart attack, in otherwise healthy adults, aged 40+, increases more than 10 times while the risk of a stroke increases more than 8 times.
Could I get the COVID vaccine/booster (3rd dose) and the Influenza vaccine this year?
According to CDC and National Advisory Committee on Immunization you can get your COVID-19 vaccine, including the booster (3rd dose) and the flu vaccine at the same time.
If you have any concerns about getting COVID-19 and the flu vaccine at the same time, you should speak with your healthcare provider.
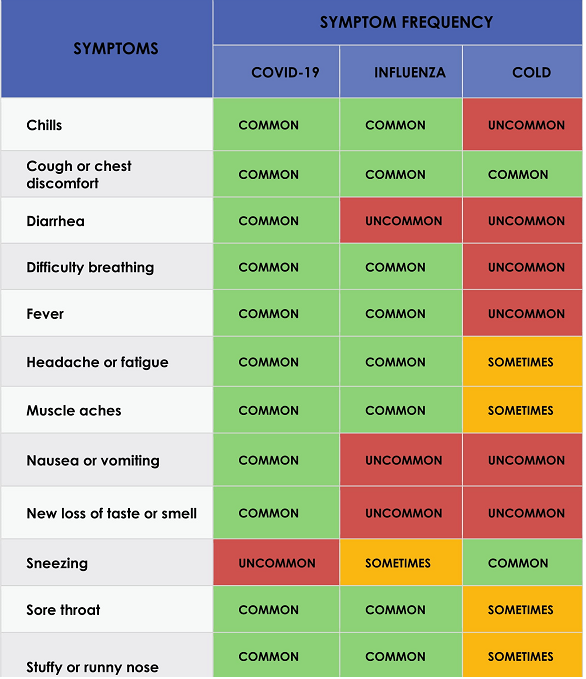
What are the common symptoms for
COVID-19, INFLUENZA, COLD?
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.
